Glioblastoma Definitions and Explanations
A glioblastoma (GBM) diagnosis can be overwhelming for patients, caregivers, and families alike. To help you navigate through this complex journey, Gray for Glioblastoma has compiled essential definitions and explanations of key terms related to GBM. This guide will support you by offering clarity on medical terms, treatment options, and potential next steps in your glioblastoma experience.
What is Glioblastoma?
Glioblastoma, also known as GBM, is a grade IV astrocytoma—an aggressive, fast-growing malignant brain tumor. This cancer typically originates in the brain or spinal cord, causing severe disruption to the normal functions of these areas. Glioblastoma is known for its rapid progression and challenging treatment options, making early diagnosis and ongoing care essential (WHO).
Depending on where glioblastoma tumors develop in the brain, the symptoms and treatment approaches can vary. Glioblastoma can occur in various regions of the brain, affecting different functions. The main regions affected include…
-
When the location of the brain tumor is the Frontal lobe it may cause difficulty with:
Concentrating or focusing attention, speaking, communication skills and language production, controlling emotions and behavior, executive functions such as making decisions, solving problems, planning and organizing, learning and remembering new information, lack of inhibition, social , impulse control and sexual behavior, weakness on the opposite side of the body from the tumor, loss of smell.
-
When the location of the brain tumor is the parietal lobe it may cause difficulty with:
bringing together information from your different senses (touch, vision, hearing, smell, taste) and making sense of it, recognizing faces or objects, co-ordinating movements, spatial awareness (judging distances and hand-eye co-ordination), speaking, understanding words, writing, reading, numbness on the opposite side of the body from the tumor.
-
When the location of the brain tumor is the temporal lobe it may cause:
Difficulty hearing, speaking, identifying and categorizing objects, learning new information, correctly identifying emotions in others, memory loss, seizures or blackouts, sensations of strange smells.
-
When the location of the brain tumor is the occipital lobe it may cause:
difficulty with vision such as identifying objects or colors, loss of vision on one side.
-
When the location of the brain tumor is the cerebellum it may cause:
Difficulty with balance, a loss of co-ordination, difficulty walking or speaking, difficulty using executive functions (making decisions, solving problems, planning and organizing) flickering of the eyes, vomiting, stiff neck, problems with dexterity (skills in using your hands).
-
When the location of the brain tumor is the Brain Stem/Spinal Cord it may cause:
Unsteadiness, difficulty walking, facial weakness, double vision, difficulty speaking and swallowing.
What is a Malignant Tumor?
A malignant tumor refers to cancerous growths that can invade nearby tissues and spread to other parts of the body. These tumors grow uncontrollably and are capable of metastasizing—spreading beyond their original location, making them more difficult to treat (Cancer.gov).
What is a cancer grade? What does grade IV mean?
Cancer grade refers to how abnormal the cancer cells appear under a microscope. Tumors are graded from roman numerals I to IV, with lower-grade tumors (I and II) growing more slowly and being less likely to grow into (invade or infiltrate) nearby tissues. Higher-grade tumors (III and IV), such as glioblastomas, grow rapidly and are more invasive, requiring more intensive treatments. Glioblastomas are always classified as grade 4 brain cancer.
What is a Biopsy?
A biopsy is a medical procedure in which a tissue sample is taken from a tumor for examination under a microscope. This process is critical for confirming a glioblastoma diagnosis and helps doctors determine the tumor's grade and specific characteristics, guiding treatment decisions.
MGMT Promoter Methylation
MGMT stands for O6-methylguanine-DNA methyltransferase. It’s a gene that produces a protein involved in repairing damaged DNA. This protein can fix certain types of damage caused by cancer treatments like chemotherapy. Tumors with MGMT promoter methylation often respond better to chemotherapy because the cancer cells are more vulnerable to the treatment. Doctors use this information to help decide the best treatment plan. You may hear “tumor is "methylated" or "unmethylated."
Recurrence
Recurrence occurs when cancer cells that were previously undetectable or believed to have been completely removed or treated start to grow again. This can happen in the same location where the cancer originally appeared (local recurrence), in nearby tissues (regional recurrence), or in distant parts of the body (distant recurrence).
Glioblastoma is known for its high rate of recurrence due to its aggressive nature and the challenge of completely removing or treating all tumor cells (Mayo Clinic). According to the Central Brain Tumor Registry of the United States Statistical Report, about 90 percent of patients with glioblastoma will experience a recurrence.
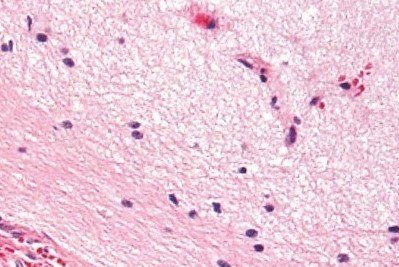
Tumor Location
“Normal brain cells”
“Glioblastoma brain cells”
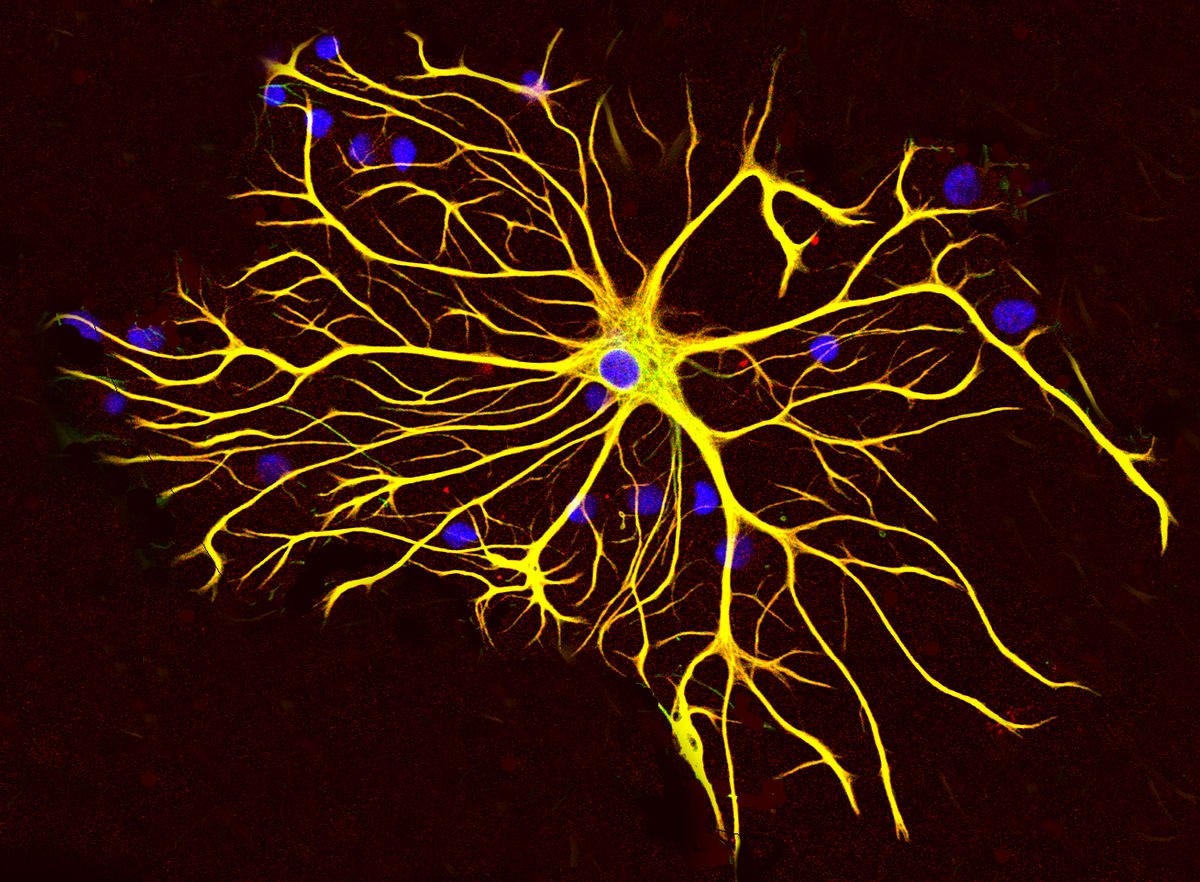
What is an Astrocytoma?
Astrocytomas are tumors that arise from astrocytes—star-shaped glial cells that make up the “glue-like” or supportive tissue of the brain (ABTA).
Steroids: Dexamethasone is the drug of choice to relieve symptoms due to the brain swelling that is often associated to the tumor. It is a very effective drug, which acts quickly and reliably. Unfortunately, it does not have any action against the tumor, and it is associated to significant side effects when used for periods longer than 2-3 weeks: weight gain, high blood sugars, hypertension, increased risk of infection, irritability.
Chemotherapy with TMZ: Temozolomide (TMZ) is a drug which is taken by mouth and works by slightly modifying the DNA of tumor cells. This effect on the DNA triggers its breakage and consequent death of the cell, unless DNA repair mechanisms override the damage. It is usually taken daily for 5 days, followed by a rest period of 3 weeks, before starting another cycle.
Radiotherapy: Radiation works by damaging DNA of the tumor cells. Under standard protocols, the treatment consists of small doses of radiation in the area of the tumor, 5 days a week for 6 weeks. Side effects are local hair loss (usually temporary), and fatigue. Long term side effects are necrosis of the brain around the treated region, and cognitive difficulties.
Bevacizumab (Avastin): Bevacizumab is a drug that blocks the tumor’s ability to recruit blood vessels so that they can feed themselves and keep growing. Avastin has been approved by the Food and Drug Administration (FDA) in 2013 for its use in recurrent glioblastomas. It is very effective in reducing the swelling associated with the tumor and often helps improving symptoms. Unfortunately, it does not significantly prolong survival.
Antiseizure Drugs: Levetiracetam (Keppra) is the most widely used drug for this purpose. It is usually reserved only for patients that have experienced tremors or seizures.
Via Mayoclinic.org
A type of procedure performed on the brain while you are awake and alert. During the procedure, doctors place your head in a fixed position to keep your head still and ensure surgical accuracy. Some of your hair may be clipped to do this. An anesthesiologist will give you some medication to make you sleepy for parts of your awake brain surgery. Your neurosurgeon will apply numbing medications to your scalp to ensure your comfort. During surgery, a team of speech-language pathologist may ask you questions or ask you to identify pictures or words on cards, make movements, count numbers or raise a finger. Your responses help your surgeon identify and avoid damage to the functional areas in your brain (Mayo Clinic).
Common Medication Names
What is a Craniotomy?
Blood-Brain Barrier
A selective permeability barrier between the bloodstream and the central nervous system. It can make delivering treatments to the brain more challenging. The BBB is a selective barrier made up of tightly joined cells lining the blood vessels in the brain. It separates the brain’s blood supply from the brain tissue itself. One of the biggest challenges with this barrier is that it can also prevent many therapeutic drugs from reaching the brain. This makes treating brain conditions, like glioblastoma, more difficult because many chemotherapy drugs and other treatments cannot easily cross the barrier. Scientists are studying ways to bypass or temporarily open the barrier to deliver treatments more effectively.